In July 2019, barely six months before the pandemic, we worked with alumni of The Geneva Learning Foundation’s immunization programme to build the Impact Accelerator in 86 countries. This global community of action for national and sub-national immunization staff pledged, following completion of one of the Foundation’s courses, to support each other in other to achieve impact.
Closing the loop from learning to impact produced startling results, accelerating the rate at which locally-resourced projects were implemented and fostering new forms of collaborative leadership. Alumni launched what immediately became the largest network of immunization managers in the world.
Then the pandemic dramatically raised the stakes: at least 80 million children under one were placed at risk of vaccine-preventable diseases such as diphtheria, measles and polio as COVID-19 disrupted immunization service as worldwide.
Alumni were amongst the first in their countries to respond, leveraging the power of being connected to each other to create a virtuous circle of peer support that became the COVID-19 Peer Hub. As a result, the pace of growth keeps increasing. Membership doubled during the summer of 2020.
The network effect cannot be replicated by smaller platforms built on top-down legacy models of the past. Nor can the trust and friendship that bind members to each other.
Members are telling their own stories of the COVID-19 pandemic, disseminating rapid learning, first about recovery of immunization services and, more recently, about COVID-19 vaccine introduction.
There is no upper limit to the number of participants or stories. Rather than painstakingly collecting a few stories so highly curated that they seem too sanitized to be authentic or meaningful, we created the conditions for each person to share their story and learn from the stories of others. We do not require you to be “exemplary” to experience or share significant learning. Some of the most powerful lessons learned, in fact, come from the experience of failure.
In November 2020, for example, members worked together to produce in just four weeks over 700 detailed, peer-reviewed case studies of vaccine hesitancy in health facilities and districts. These were used to inform the COVID-19 Peer Hub’s early scenario planning for vaccine introduction and are now being analyzed for the unique insights they contain, available by no other means.
These stories are about collaboration and learning from each other, within and across borders and all levels of the health system, in new ways to do new things required to face the pandemic. I do not believe it is an overstatement to say that participants are writing history.
Co-design as a networked practice of continuous invention, innovation, and learning
For COVID-19 vaccine introduction to succeed, we need new ways to disseminate rapid learning. Through co-design with members of our platform, we invented two in the first three months of this year: Teach to Reach: Connect and the COVID-19 Peer Hub Inter-Country Learning Collaborative to support vaccine introduction.
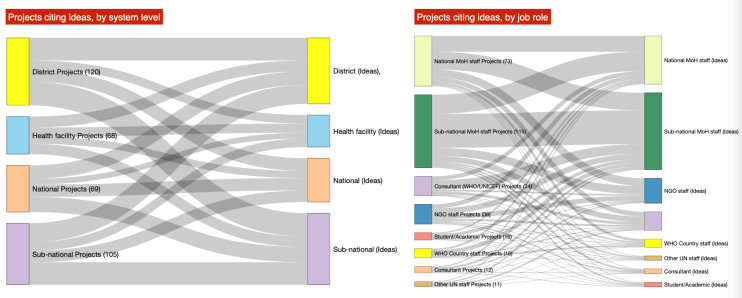
We already knew that presentation webinars do little more than replicate classroom training in a digital format. Yet they proliferate, despite the dearth of evidence about their effectiveness, with unsubstantiated claims that they are somehow “collaborative” or that 10 minutes of attendees asking the experts a few questions qualifies as “peer learning”. Social Network Analysis (SNA) of the COVID-19 Peer Hub by Sasha Poquet and Vitomir Kovanovic at the Centre for Complexity and Change in Learning helped us to understand that the power of the network lies in the relationships between its members, not only in our ability to convene or call to action, and certainly not in one-way information transmission.
So, on Friday 26 March 2021, 1,372 immunization professionals attended Teach to Reach: Connect to meet, network, and learn about COVID-19 vaccine introduction, how to improve immunization training, and how to reach “zero-dose” children. The feedback received from participants has been incredible, starting with their own surprise that they had so much to learn from each other. (You can catch the opening ceremony on our YouTube channel, and we will soon be sharing what we learned in upcoming live-streamed events on our Facebook page.)

An inter-country peer learning collaborative to accelerate COVID-19 vaccine introduction
The next day, the COVID-19 Peer Hub team from the Democratic Republic of the Congo (DRC) invited their colleagues from Ivory Coast to learn from the latter’s experience of vaccine introduction. Participants compared the enthusiasm to that for a football match, only this time, they said, the purpose was to “kick out the Coronavirus”. The meeting, hosted by DRC Peer Hub team leader Franck Monga and facilitated by a brilliant young doctor from Burkina Faso, Palenfo Dramane, drew over 1,000 attendees from 20 francophone countries. Panelists from Ivory Coast were alumni of Foundation programmes directly involved in vaccine introduction, working at various levels of the system. They shared first-hand experience from the first few weeks of vaccine introduction. Attendance barely declined even though the meeting ran over time by more than 90 minutes.

Our ‘grand challenge’
Our biggest challenge, so far, has been to explain the power, significance, potential, and value of such events to our global partners. This is ironic given that the global immunization community agrees that it is sub-national immunization staff who make the difference needed to achieve Immunization Agenda 2030, the new strategy adopted last year by the World Health Assembly. Some global colleagues did take the time to apologize, explaining that they were too busy on Friday afternoon due to COVID-19 vaccine introduction to take 15 minutes to meet, network, and learn with immunization staff from the countries they serve and who are actually introducing the vaccine. (To be fair, a few colleagues did attend and loved it.) Last but not least, donors remain risk-adverse, preaching innovation while repeatedly choosing conventional approaches and traditional partners, even when they have failed in the past, seemingly driven by considerations other than scale, results, or demand from countries. In some cases, they have even expressed disbelief, doubting our results as too good to be true, flummoxed by how a new entrant with limited immunization experience could achieve them when better-funded, far-more-legitimate institutions have simply not been able to do so.
